A Complete Guide to Pudendal Neuralgia
Contents
What is Pudendal Neuralgia? Where Does the Pudendal Nerve Run? What Triggers Pudendal Neuralgia? How to Recognize Pudendal Neuralgia? Which Specialist to See for Pudendal Neuralgia? What Are the Treatments for Pudendal Neuralgia? How to Live with Pudendal Neuralgia? TestimonialsWhat is Pudendal Neuralgia?
Pudendal neuralgia, also know as pudendal nerve entrapment, is defined by the following:
- • Damage to or compression of the pudendal nerve causing inflammation
- • Pain in the perineal region
- • Difficulty or inability to remain seated
While women represent the majority of cases (7 out of 10), pudendal neuralgia is estimated to affect 6.6% of the general population. It most commonly develops between the ages of 50 and 70, but people of all ages can be affected.
Where Does the Pudendal Nerve Run?
The pudendal nerve innervates the perineal region—between the genitals and the anus.
Its path begins at the base of the brain and continues through the spine to the sacrum in the pelvis. From there, it passes under the piriformis muscle and between the sacrotuberous and sacrospinous ligaments. It then runs through Alcock’s canal, giving the condition its alternate name: Alcock’s canal syndrome.
Inside Alcock’s canal, the nerve branches off into the rectal nerve and other extensions that supply:
- • the scrotum or labia
- • the penis or clitoris
- • part of the levator ani muscles, the ischiocavernosus and bulbospongiosus muscles, and the bulb of the penis

What Triggers Pudendal Neuralgia?
Possible Causes of Pudendal Neuralgia
There are many ways pudendal neuralgia can develop, making it challenging to diagnose. While not all causes are fully understood, common triggers for pudendal nerve pain include:
- • Following surgery
- • After childbirth
- • Internal compression (e.g., inflamed bladder)
- • Direct nerve injury (neuropathy)
- • Falls that cause compression or bruising near the nerve
- • Chronic pressure on the pudendal nerve, such as from intense cycling or prolonged sitting
How to Recognize Pudendal Neuralgia?
Recognizing Symptoms of Pudendal Neuralgia
Pudendal neuralgia is often mistaken for gynecological or urinary disorders due to the intimate and painful nature of the symptoms. This confusion, along with the term "shameful nerve," makes it a difficult condition to discuss.
Common Symptoms of Pudendal Neuralgia
Symptoms typically affect the genitals, anus, rectum, and urinary system. To diagnose pudendal neuralgia, specialists often rely on criteria such as:
- • Pain in the perineal area (anus, penis, or clitoris)
- • Pain worsens when sitting, relieved on a toilet seat (due to decompression)
- • Pain does not wake the patient at night
- • No numbness in the affected region
- • Positive response to a nerve block test
These criteria help build a diagnostic foundation, but pudendal neuralgia remains complex and varies from person to person.
Based on our experience with patients, the most reported symptoms include:
- • Burning sensations
- • Stabbing or knife-like pain
- • Sensation of a foreign object in the rectum or vagina
- • Constipation and incontinence (as the pudendal nerve transmits the urge to urinate)
Pudendal Neuralgia in Men
In men, pudendal neuralgia may affect erectile function since the pudendal nerve also controls muscles involved in erection.
Pudendal Neuralgia in Women
In women, pudendal neuralgia typically causes pain in the vulva, clitoris, and vagina. Women represent around 70% of diagnosed cases. Some studies suggest a link between endometriosis and pudendal nerve irritation, with symptoms worsening during the menstrual cycle.
Which Specialist to See for Pudendal Neuralgia?
The Role of a General Practitioner
When dealing with pudendal neuralgia, early diagnosis is key. The sooner the condition is identified, the sooner appropriate strategies can be implemented to manage symptoms and improve quality of life.
Many people first consult a general practitioner. However, pudendal neuralgia is sometimes poorly understood by some GPs. Some are unaware of the condition altogether, while others may dismiss symptoms as psychological. This lack of recognition can worsen the patient’s sense of isolation and delay proper care. Because of the lack of knowledge, it is estimated that it takes up to 4 years to diagnose a pudendal neuralgia.
Although your GP may be the first step, a pudendal neuralgia specialist can provide more targeted expertise and accurate diagnosis of Alcock’s canal syndrome.
Which Specialist Can Diagnose Pudendal Neuralgia?
The first step is often a block test performed by a neurologist. This involves injecting an anesthetic into the pudendal nerve. Temporary pain relief confirms that the nerve is the source of pain.
Additional exams may include:
- • Electromyography (EMG) of the perineal floor
- • Pelvic or spinal imaging to rule out other causes
What Are the Treatments for Pudendal Neuralgia?
Medication and Injections
Medication can help relieve symptoms but does not address the root cause of pudendal neuralgia. Injections such as anesthetics or Botox into the pudendal nerve may also help reduce pain temporarily.
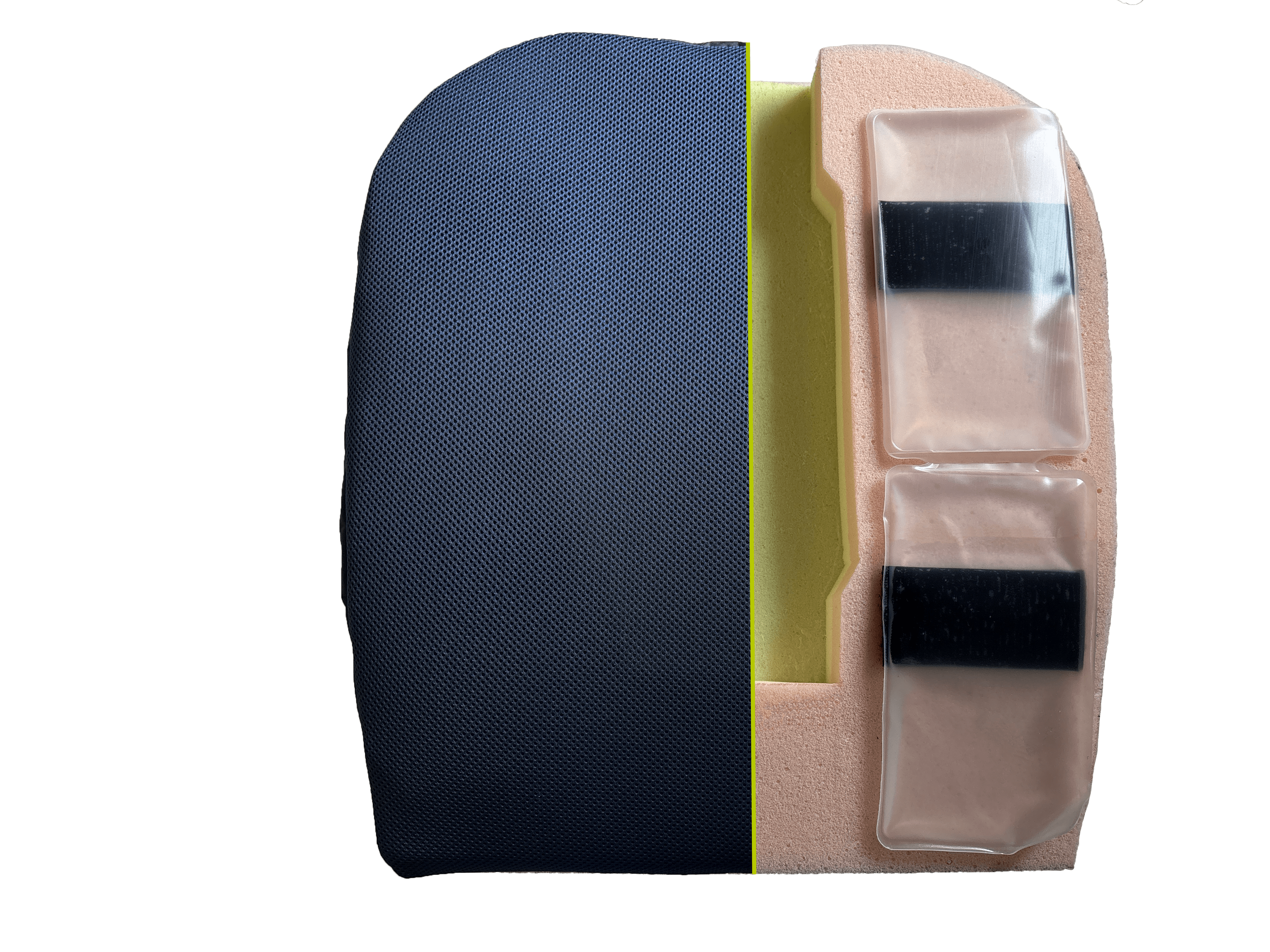
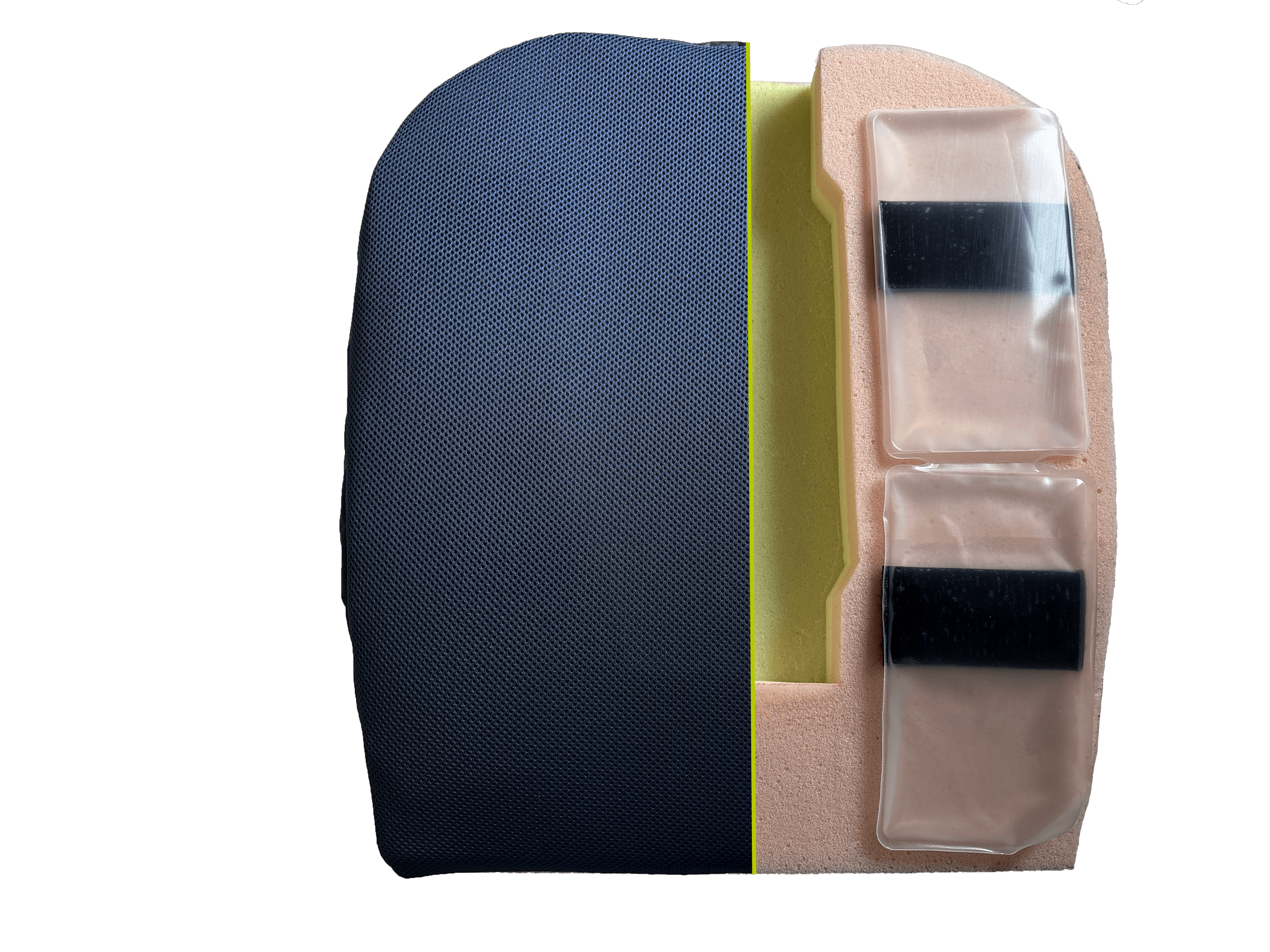
Seat Cushions for Pudendal Neuralgia
Specialized seat cushions are often effective in reducing pressure on the pudendal nerve while sitting. Our Alcock Rest seat cushion was developed based on years of research and user feedback.
Key benefits:
- • Forward tilt to promote posture and reduce abdominal and nerve compression
- • Central cut-out to relieve pressure on the perineal and coccygeal areas
- • Four High Viscosity Fluid pockets to absorb pressure and vibrations, adaptable to each user
- • Removable pockets can be chilled for a cooling pain-relief effect
Each pudendal cushion can be customized based on individual body shape and pain level.
Physical Therapy and Osteopathy
Physical therapy and/or osteopathy may be beneficial in managing symptoms. However, caution is necessary: certain movements or stretches can worsen nerve irritation.
Surgical Treatment
Surgery is a last-resort option when other treatments fail. The goal is to release the pudendal nerve from compression.
- • Transgluteal approach (through the buttock)
- • Balloon method (inserting and inflating a balloon to relieve pressure)
Results vary and must be evaluated carefully.
Alternative and Complementary Therapies
Some individuals try acupuncture, homeopathy, or herbal treatments to reduce stress and support medical care.
How to Live with Pudendal Neuralgia?
Recognition and Available Support
Currently, pudendal neuralgia is not automatically recognized for long-term illness support (ALD). However, petitions exist to advocate for better recognition of this condition.
You can apply for disability worker status (RQTH) through your local MDPH office. Note that processing times can exceed six months depending on your region.
Daily Life Tips to Relieve Pain
Our day-to-day exchanges with patients have helped us identify some practical advice:
- 1. While sitting, keep your knees slightly below your hips to adopt a "dynamic" posture and reduce nerve compression.
- 2. Limit sitting to a maximum of 2 hours at a time to prevent tension and friction.
- 3. Engage in suitable physical activity: listen to your body and avoid anything that worsens symptoms (e.g., running for some).
Adapt your posture, movements, and routines based on how your body responds to avoid aggravating symptoms.
Testimonials
Personal Experiences with Pudendal Neuralgia
Many personal stories are shared online by those living with Alcock’s canal syndrome. Associations, forums, and support groups provide opportunities for sharing and emotional support.
One Helpful resource:
- • Pudendalsite: research and shared experiences from sufferers
This platform and others offer valuable information to better understand the condition and break the isolation many patients feel.
We hope this article helps raise awareness and support those affected by pudendal neuralgia. The information is general and may vary by individual case. Feel free to share your own story to contribute to the community’s understanding.
You can also access a summary of this article via our Infographic on Pudendal Neuralgia.