Pudendal Neuralgia: Answers to the 10 Most Frequently Asked Questions
Posted by
Marion Bihoué
Jan 20, 2025
Neuralgia
Comments
0

Pudendal Neuralgia: Answers to the 10 Most Frequently Asked Questions
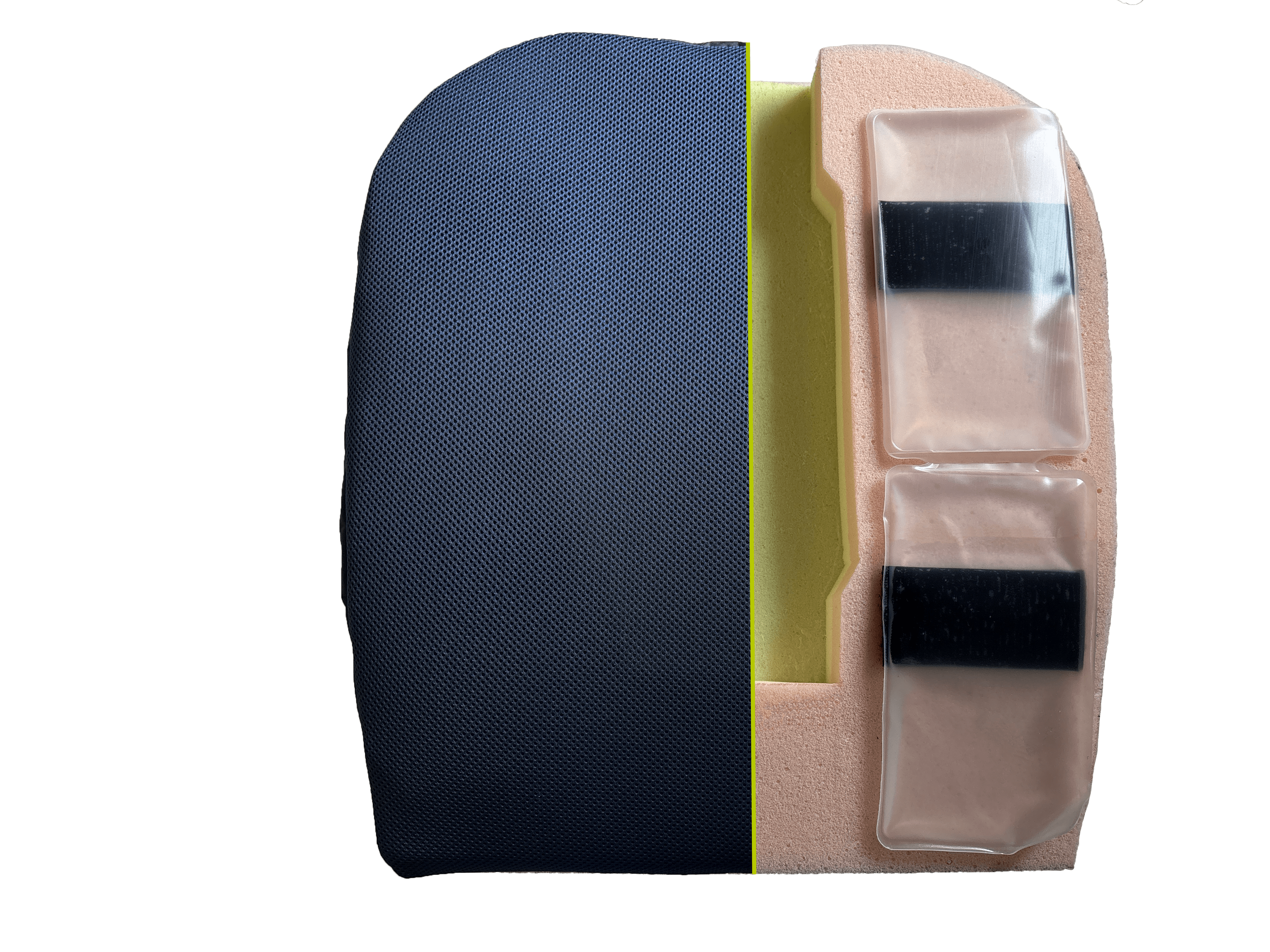
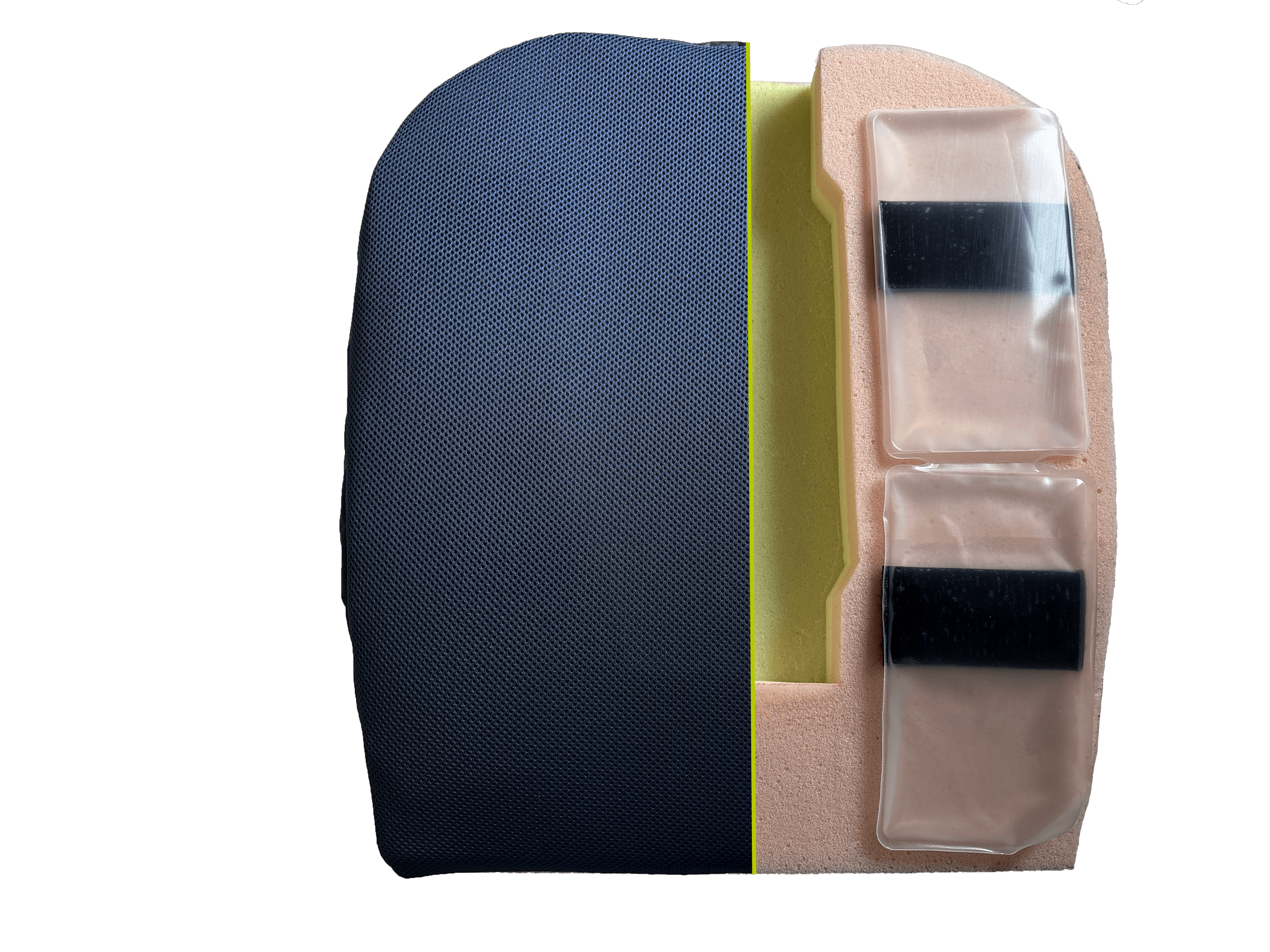
Discover our pudendal neuralgia seat cushion
▶ What is Pudendal Neuralgia?
▶ Where Does the Pudendal Nerve Run?
▶ What Triggers Pudendal Neuralgia?
▶ What Are the Symptoms of Pudendal Neuralgia?
▶ Which Tests to Diagnose Pudendal Neuralgia?
▶ Is it Possible to Cure the Pudendal Nerve?
▶ Which Specialist Should I See for Pudendal Neuralgia?
▶ How to Live Daily with Pudendal Neuralgia?
▶ Are There Support Groups or Forums for Pudendal Neuralgia?
▶ What Aids and Support Are Possible for Pudendal Neuralgia?
For more information on causes, symptoms, and treatment options, visit our blog dedicated to pudendal neuralgia.